Uganda
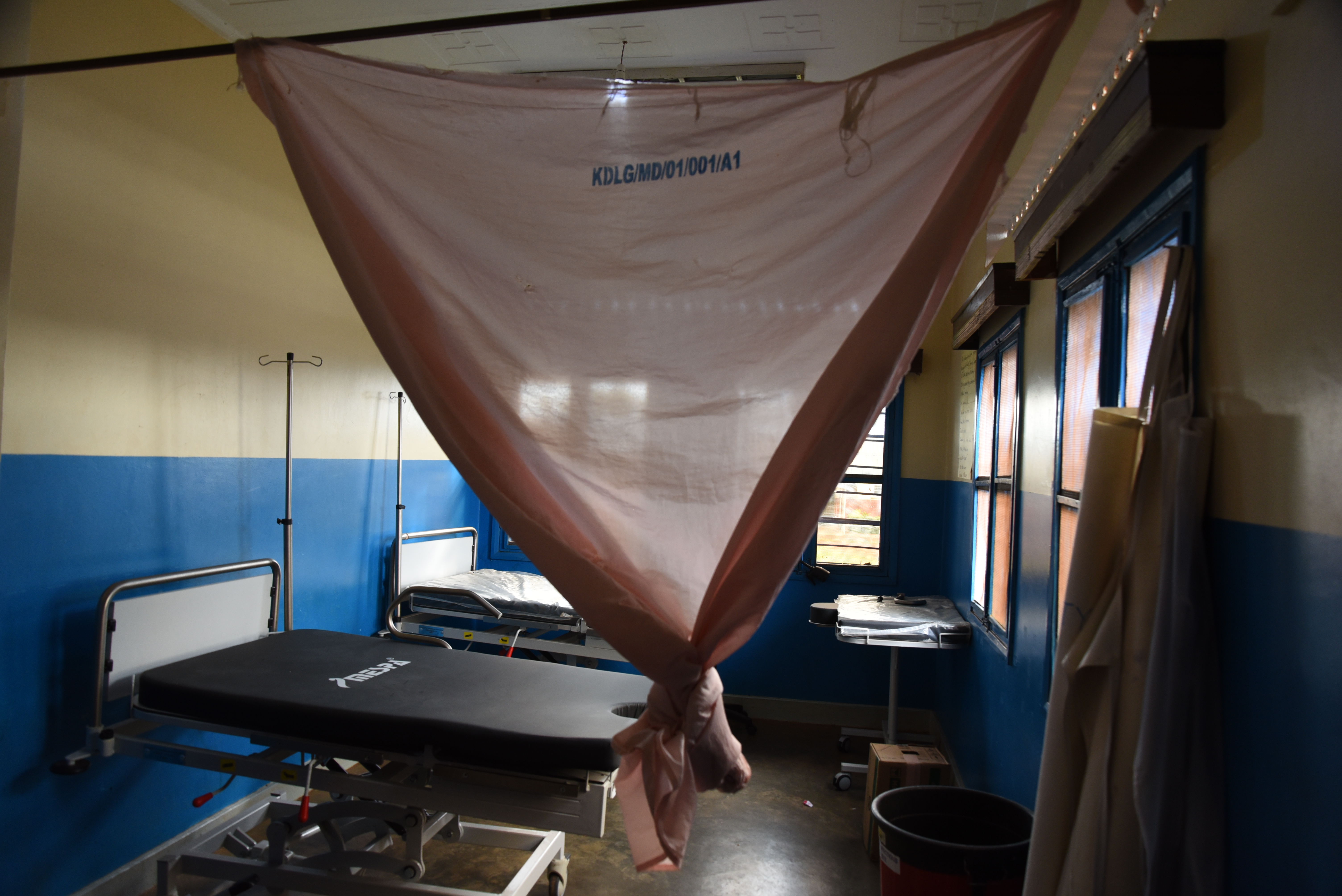
Kamuli Referral Hospital
In partnership with HOLD Uganda, in June 2018, we did a site visit to the Kamuli Referral Hospital. We applied the Saving Mothers model to employ low-cost solutions to make high- impact, sustainable reductions in maternal mortality in this low-resource setting.
What we learned
Uganda has persistently high maternal and neonatal mortality. In the Kamuli District in particular, there is a major lack of physicians (3/500,000) and consequently nurse midwives de facto are the most skilled providers at Kamuli Referral Hospital. TBAs (Traditional Birth Attendants) are common, and due to the high volume of home births are often the only people to assist during childbirth. VHTs (Village Health Team workers) work on the frontlines of primary care in their communities and have a recognized role in the health care system. Through quantitative and qualitative methods, we determined that nurses have solid diagnostic skills but have not been empowered to provide definitive care. We tailored their training curricula to fill these gaps in education by focusing on clinical management of complications.
Response
We are piloting a Skype-based telemedicine curriculum to meet the needs of nurses, midwives and health educators in Kamuli, Uganda. Each lecture is case-based and capped with a facilitated discussion to gauge understanding and apply lessons learned. Topics range from postpartum hemorrhage management and preeclampsia/eclampsia to twin pregnancies and ultrasound use. Each session is bookended by assessment forms to track progress and areas of improvement for both instructor and student. Ultimately, this lecture series builds a sustainable partnership with our team in Uganda and empowers local health workers to address the maternal health issues facing their community.
Our work in action
Saving Mother's summer intern (2018) Marga Kempner captured our experiences on ground